Basketball players are notoriously tough on their feet. In this blog post, we look at some common basketball foot and ankle injuries and some conservative treatment approaches.
- Note: Correct Toes® does not provide medical advice, diagnosis, or treatment. The content contained in this website is for educational or informational purposes only and is not intended to replace or augment professional medical instruction, diagnosis, or treatment. Do not ignore professional medical assistance or avoid seeking treatment for your health problems due to something you have read or viewed on this website. Schedule an appointment with your primary care provider if have any questions about medical conditions or your health status.
- Correct Toes are used and loved by several NBA, NFL, and NCAA teams for both injury recovery and prevention as well as training purposes.
Minor Injuries
Blisters – occur when the outer layer of skin separates from the inner layer of skin and the space between these layers fills with lymph fluid. They are usually caused by friction from shoes that are too tight, inappropriately shaped (narrow toe boxes), or ill-fitting, rubbing repeatedly against the skin.
- – Treatment: Prevention is paramount. Wearing natural, foot-shaped shoes with a wide toe box that fits your foot well and moisture-wicking toe socks will help to prevent blisters. Use synthetic wicking socks or socks made from natural fibers like wool or bamboo; discontinue and avoid cotton socks as they retain moisture. Consider double-layered socks to reduce friction. Change socks often when in footwear for prolonged periods or immediately following exercise. Consider applying topical drying powders (cornstarch- or arrowroot-based, talc-free) as needed. Use tape, moleskin, or various hydro gels for existing blister. See this video by Dr. Ray McClanahan for more information about treating and preventing blisters.
Corns and Calluses – buildup of thick, hardened skin caused by prolonged pressure or friction on the skin. A corn is thickened skin on the top or sides of the toes, often caused by narrow toe boxes; whereas a callus is thickened skin on the soles of the feet, typically under the metatarsal heads, often caused by toe spring and heel elevation. Calluses that develop a painful core or seed inside of them are known as intractable plantar keratosis (IPK). IPKs are generally located under the metatarsal heads and are frequently misdiagnosed as plantar warts.
- – Treatment: Wearing natural, minimal footwear with a wide toe box and flat sole will help to prevent rubbing which causes the corns and calluses. Reduce the thickness of corns or calluses by filing or trimming with a pumice stone or emery board. Consider double-layered socks to reduce friction. Topical over-the-counter acid plasters can be used to assist eroding especially thick corns and calluses, although use with caution as acid is capable of damaging the surrounding healthy tissue. Avoid using acid plasters if you have diabetes, nerve-related conditions and/or poor circulation. See this video by Dr. Ray McClanahan for more information on treating corns and calluses with conservative care.
Bruised and Ingrown Toenails – pressure and friction from shoes that are too tight with narrow toe boxes cause the edge of the toenail to grow into the toe’s skin, causing pain, redness, and swelling near the nail.
- – Treatment: The most important conservative care technique in preventing ingrown toenails is avoiding toe spring, heel elevation and tapering toe boxes when selecting footwear, as these features all increase pressure along the toes and toenails. Naturally shaped footwear possesses a toe box that is widest at the ends of the toes and allows all toes to spread. Spreading the toes allows offloading and reduction of pressure along the toenails. which reduces the risk of nails pressing and rubbing along skin, decreasing likelihood of nails becoming ingrown. See this video by Dr. Ray McClanahan for more information on treating ingrown toenails with conservative care.

Athletes Foot and Fungal Toenail Infection – tinea pedis typically develops on the bottom of the foot and between the toes. Fungi normally live on many surfaces, including the skin, and what makes a person become infected is typically genetic susceptibility and reduced immunity in combination with a warm, dark, moist foot environment in which fungi thrive. When the toenail becomes damaged, the fungal infection can spread under the toenail. Wearing closed-toe shoes that compress or squeeze the toes, increasing friction and mild skin breakdown and keeping the feet wet for prolonged periods can result in fungal infection. This condition can be difficult to treat and may recur following treatment
- – Treatment: One of the most important factors in treating and preventing athlete’s foot is creating an environment that is light and dry, not dark, warm, and damp. Limiting exposure to enclosed footwear will aid in skin recovery; consider going barefoot more often or wearing sandals in place of closed-toe shoes as much as possible to create a foot environment in which fungi cannot thrive; UV light is a potent aid in combating fungal infections. When enclosed footwear must be used, make sure shoes are naturally shaped to limit toe rubbing and constriction. Use synthetic wicking socks toe socks, or wear socks made from natural fibers like wool or bamboo and change socks often when in footwear for prolonged periods, or immediately following exercise. Discontinue and avoid cotton socks, as cotton fibers retain moisture and use a shoe dryer to dry footwear after prolonged use. File, trim, and thin out thickened nails and apply over the counter topical medications nightly to dry/clean skin and nails. Cover with saran wrap/plastic to aid penetration of the substance into infected skin. Consider applying topical drying powders (cornstarch- or arrowroot-based, talc-free) as needed.
Chronic and Over-Use Injuries
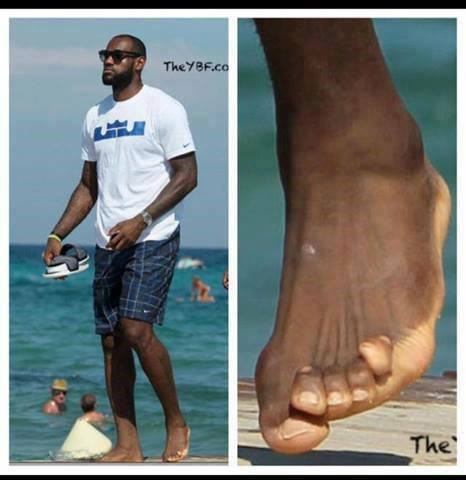
Bunion – medically known as hallux abductovalgus, a condition in which the big toe and first metatarsal bone (the long bone located directly behind the big toe, extending to the midfoot along the medial arch) are displaced, exposing the head of the first metatarsal bone. The ‘bump’ of the bunion is not a growth of bone, but rather the exposed first metatarsal head, as the big toe shifts towards the second toe. The resulting shift of the first metatarsal widens the ball-of-the-foot and destabilizes the midfoot and may become reddened and enlarged when compressed in footwear. Pressure from footwear may irritate the skin or cause additional soft tissue enlargements as the body tries to protect the displaced bone. While there is heritable disposition to bunion formation, the underlying cause of bunions is narrow, tapered toe boxes.
Note: A tailor’s bunion (bunionette) is a bunion on the 5th toe (pinky).
- – Treatment: The first and most important step in the conservative and natural management of bunion formation involves a departure from conventional footwear and toward naturally shaped footwear. Avoid toe spring, heel elevation, and tapering toe boxes when selecting footwear. Correct Toes, our anatomical toe spacer, helps to align, strengthen, and restore toe function. Also consider range of motion exercises that relocate the big toe such as the bunion stretch and soft tissue release. See this video by Dr. Ray McClanahan for more information on treating bunions with conservative care.
Hammer Toes – a hammer toe is both flexed slightly up into dorsiflexion at the metatarsal-phalangeal (MTP) joint and also flexed down into plantarflexion at the first toe joint, or proximal interphalangeal (PIP) joint. The development of hammer toe formation is slow, typically occurring over years and decades. Inappropriate footwear is the most significant factor in the development of hammertoes. Shoes that are too narrow in the toe box force the toes into a curled and deformed position. Shoes with an elevated heel shorten the calf muscles, including the extensor and flexor muscles that insert on the toes, pulling the toes back into the hammer toe shape. Over time, the toe tendons adjust to this unhealthy configuration, causing the toes to hold a hammered shape. Athletes may be especially susceptible because of the increased forces on the toes from shoes that are too small or too tight. Heel elevation in footwear is also problematic, as it causes the toes to be pushed into the shoe’s toe box as well as contributing to a muscle/tendon imbalance in the foot and toes.
- – Treatment: Again healthy, natural footwear is the place to start. Shoes without heel elevation, without toe spring, and with wide toe boxes allow the feet to be flat on the ground with the toes splayed wide. Correct Toes can also aid the recovery of mobile hammertoes by placing force over the PIP joint to encourage the toe to lengthen and lay flat. Metatarsal Pads are a great tool that can be placed inside shoes that will encourage top-of-foot lengthening and relaxing. Stretching exercises like the toe extensor stretch or hammer toe stretch can be very beneficial in reshaping the soft tissue to allow for hammer toes to return to lying flat. See this video by Dr. Ray McClanahan for more information on treating hammer toes with conservative care.
Capsulitis – inflammation of the joint capsule, typically at the second MTP joint. Heel elevation, toe spring, and tapered toe box combine to put the foot in an injurious position, shifting the body weight onto the ball of the foot, putting excess pressure onto the extended and exposed MTP joints. A low heel will shift the 60% of the body weight to the ball of the foot and a high heel can shift up to 90% of body weight onto the ball of the foot. Simultaneously, this extended position displaces the plantar fat pad, that normally sits under the MTP joints for comfort and protection, distally towards the toes, further exposing the MTP joints. When friction, improper movement, and excessive pressure is applied the MTP joints, the joint capsule becomes inflamed and painful.
- – Treatment: Beyond rest, transitioning to natural, healthy footwear, avoiding toe spring, heel elevation, and tapering toe boxes, will be the most beneficial conservative long-term treatment.. Correct Toes will help to realign the toes and metatarsals to their correct anatomical position. Metatarsal Pads can be placed inside shoes and will encourage top-of-foot lengthening and relaxing, repositioning the toes and plantar fat pad into healthy alignment. Stretching exercises like the toe extensor stretch will be extra helpful to reshape the foot to be flat on the ground. See this video by Dr. Ray McClanahan for more information on treating capsulitis with conservative care.
Shin Splints (Tibial Fasciitis) – involves pain along the inner edge of the shin bone, commonly manifesting during or following vigorous physical activity. Tibial fasciitis occurs when physical activity, typically jumping and landing, causes lower leg muscles to pull on the periosteum, irritating the innervated and vascularized dense layer of connective tissue that encases bone. Both the elevated heel and toe spring features of common athletic shoes will contract and shorten lower leg musculature. Paired with a tapered toe box that destabilizes the midfoot, all lower limb muscles are forced to function outside of their ideal anatomic alignments and length-to-tension ratios. Additionally, rigid soled footwear prevents the natural motion of the foot arches. In a normal, mobile foot, decreasing arch mobility hinders muscle contraction and leads to atrophy of foot muscles. This limits the ability of the arches to absorb impact and produce energy for the next step. Lower limb muscles along the shin bone that insert and act upon the foot will still contract, but the foot will be unable to respond or move within its rigid environment. This results in more force acting upon the tibia as muscles try to contract and move, creating sheering and torque.
- – Treatment: It’s probably a good idea to give your legs a rest and possibly re-evaluate your training program. Choose naturally shaped footwear with a wide toe box, no heel elevation or toe spring, and a flexible sole without support features. Spreading the toes with the use of Correct Toes allows the calf deep flexor muscles and anterior extensors to engage more fully and be balanced in length-to-tension relationships; this foot and toe position helps optimize circulation for all lower limb muscle compartments. Metatarsal pads and toe extensor stretches can help especially with anterior tibial fasciitis. Also consider compression stockings and a topical heating sports cream. See this video by Dr. Ray McClanahan for more information on treating shin splints with conservative care.
Sesamoiditis – Sesamoid bones are “floating bones” within the flexor hallucis longus tendon on the bottom of the foot, which flexes your big toe. Narrow toe boxes displace the big toe inwardly, pulling this tendon, and thus the sesamoid bones, towards the midline of the foot. When in the correct position the sesamoids act as pulley, like the kneecap, however, can cause pain and limit range of motion when displaced. Additionally, an elevated heel will displace body weight onto the ball of the foot, putting extra pressure onto the first MTP where the sesamoid bones are located; and a toe spring will displace the plantar fat fad further exposing the sesamoids.
- – Treatment: Naturally shaped footwear possesses a toe box that is widest at the ends of your toes and allows all the toes to spread, an action that can be further enabled with the use of Correct Toes, which helps to correctly reposition the big toe. See this video by Dr. Ray McClanahan for more information on treating sesamoiditis with conservative care.

Plantar Fasciosis – commonly mistakenly called plantar fasciitis, is actually more accurately termed plantar fasciosis because the tissue involved is actually a collection of dead tissue, and not active inflammation. Rigid toe spring combined with heel elevation causes the muscles under your foot, your flexors, become excessively stretched and weakened, while your extensors, on top of your foot, become too tight. Additionally, tapered toe box and toe spring causes the flexor retinaculum and abductor hallucis muscle on the medial aspect of the foot to become taut from over-extension and compresses the posterior tibial artery. The blood flow to the plantar fascia becomes compromised by the position the foot is held in and this lack of blood flow causes parts of the plantar fascia to die and become necrotic and fibrotic.
- – Treatment: Look for minimalist, healthy footwear with a wide toe box and flat and flexible sole. Spreading the toes with the use of Correct Toes allows the calf deep flexor muscles to lengthen and engage more fully, offloading stress on the plantar fascia. Natural foot and toe position help optimize circulation in the foot tissues, encouraging removing of fasciotic accumulation and delivery of oxygen to plantar fascia tissue. Metatarsal Pads and stretches like the toe extensor stretch will encourage top-of-foot lengthening and relaxing of the plantar fascia. See this video by Dr. Ray McClanahan for more information on treating plantar fasciosis with conservative care.
Achilles Tendinopathy – characterized by collagen degeneration, not inflammation, most commonly occurring at the point where the Achilles tendon attaches to the heel bone or less than 1 inch above this point. Most conventional basketball shoes are designed with more cushion at the heel, lifting the heel up. This decreases the Achilles tendon functional length, changing structural integrity and length-to-tension relationships of several posterior calf muscles. In addition, shoes that are too short in heel-to-toe length or shoes with a heel counter may rub and cause pain. Rapid increasing training volume or intensity and/or transitioning too quickly from shoes with heel elevation to shoes with little heel elevation may cause Achilles tendinopathy. This transition provokes the Achilles tendon to adapt and stretch up to 1 inch in length and the stretching forces along the Achilles tendon pull at the insertion point, causing irritation and pain.
- – Treatment: A slow, gradual transition to natural, healthy footwear with minimal heel elevation that allows the foot to splay flat is the first place to start. This will place all the lower leg muscles back into their natural length-to-tension relationship. Spreading the toes with the use of Correct Toes allows the calf deep flexor muscles to engage more fully, off-loading the Achilles tendon. This foot and toe position helps to optimize circulation in the foot tissues and encourages a balance in tissue tone between your toe flexor and extensor muscles/tendons. Eccentric stretching and strengthening will also help to rehabilitate the Achilles tendon.
Stress Fractures – overuse injuries that occur when foot muscles become fatigued and are no longer able to absorb the shock of footfalls. When the foot muscles are unable to effectively absorb the shock of prolonged and repetitive foot strikes, the stress forces are then transferred to bone, which can lead to the formation of a small crack in one of the weight-bearing bones of the lower leg or foot. Basketball players and long-distance runners who wear conventional running shoes are particularly susceptible to this type of injury. Wearing shoes that deform the foot and have cast-like support features, like a rigid sole with arch support, narrow toe spring, and heel elevation, will weaken and atrophy the muscles and joints within the foot. An athlete needs their muscles, joints, and arches to be strong and to act like a natural spring, yet artificial arch support significantly restricts that spring-like function. This lack of movement keeps your feet from working under their own natural power and these now weaker muscles lack stamina and tire at an accelerated rate, putting additional pressure onto the bones. Artificial arch support also encourages improper alignment and weight distribution, displacing additional stress onto the bones. Common symptoms associated with foot stress fractures include pain, tenderness, and swelling in the involved area during physical activity. Stress fractures typically occur in the lower leg and foot. Of all the fractures that occur in the NBA, the metatarsal stress fracture is the most frequent, followed by tibial stress fractures and navicular stress fractures. X-rays of the injured area typically do not reveal evidence of a fracture until the fracture begins to heal two to three weeks after the injury occurred.
- – Treatment: Suspected stress fractures should be treated with six to eight weeks of rest. Crutches can be helpful in some cases. One can reduce the risk of a stress fracture by balancing a certain level of weight bearing loading in the off-season with the need to recover from the season’s stress level as well. Consider participating in non-basketball related activities during the off-season to avoid over-use. Slowly transitioning to natural, healthy footwear without support features will help to strengthen the muscles and joints in the foot. Correct Toes will help to anatomically realign the foot bones and joints into a healthy position to function as nature intended. Foot exercises to strengthen the intrinsic foot muscles will help to protect the foot bones and joints and prevent stress fractures.

Acute Injuries
Strains and Sprains – very similar injuries with similar symptoms. In both cases the athlete experiences pain, swelling, and limited range of motion. A strain is an injury to contractile tissue, i.e. overstretched or pulled muscle, muscle tear, tendon tear. Tendons are the attachment sites of muscles onto bone and you are more likely to experience muscle spasm and cramping with strains. A sprain is an injury to non-contractile tissue, i.e. overstretched ligament or ligament tear. Ligaments are the bands of tissue that connect 2 bones together in a joint and you are more likely to experience bruising with sprains.
- Ankles – Ankle sprains are the most common injury in the NBA, affecting approximately 26% of NBA players over the course of a single season, accounting for a large number of missed NBA games. The majority of ankle sprains are inversion sprains to the lateral ligaments, typically the anterior talofibular ligament and the calcaneofibular ligament. A narrow, tapered toe box will squeeze the toes inwards towards the midline of the foot, which drastically destabilizes the foot and ankle, collapses the medial foot arch, and leads to overpronation. Wide, splayed toes help to prevent excess eversion and inversion of the ankle. A heel elevation causes the lower leg bones (tibia and fibula) to sit further back on the posterior part of the ankle bone (talus), where it is narrower and this position is much less stable, increasing the chances for an ankle injury. Heel elevations also shorten and stiffen the calf muscles and tendons, negative impacting performance and leaving them more vulnerable to injury.
- Knees – as the joints directly above the ankles, the knees are next in line to be affected by foot and ankle instability. Heel elevations cause a compensatory change in the position of the knees to chronically increased knee flexion. This position, over time, creates increased contractile forces upon the quadriceps muscles, increased pressure on the knee joint, and chronic contraction of the hamstrings, resulting in knee pain from patellofemoral syndrome and shortened hamstring muscles. Additionally, the combination of tapered toe box, rigid toe spring, and elevated heel combine to cause an overpronation of the ankle, leading to an excessive internal rotation torqueing force at the knee. These excess forces exposed to the knees by way of unhealthy footwear displacing the forces from the feet and ankles, results in many knee injuries, particularly the ACL and meniscus.
- Low back – just like the knees, the low back and pelvis will also compensate for features of unstable footwear, heel elevations in particular. As heel elevations translate the body’s center of gravity anteriorly, the pelvis tilts forward and the spine arcs posteriorly in a lordotic curve to recapture some balance and alignment. This position shortens and tightens the hip flexors and the lumbar muscles, which then become more vulnerable to injury. Excessive cushioning in shoes can also play a role in improperly redistributing impact forces to the knees and low back.
- – Treatment: First and foremost, rest. For immediate pain, consider acetaminophen (Tylenol), which is not an NSAID, as it will help to relieve pain without inhibiting inflammation. Acute inflammation is a healing response and shouldn’t be suppressed. Additionally a topical heat-based sports cream can help to reduce pain. Although ice can help to numb pain, we don’t recommend ice long-term because it constricts blood vessels and slows the healing process. Alternatively, heat helps to dilate the blood vessels so the body can more quickly bring in healing precursors and clear away debris. For swelling, consider elevating the foot above the level of the heart and wearing a compression sleeve. Swelling is initially part of the healing response, but sometimes needs some assistance reducing as it is easy for fluid to accumulate in the foot due to gravity and posture. Supplements like Ligament Restore by Pure Encapsulations, which contains collagen, glucosamine, chondroitin, hyaluronic acid, vitamin C, lysine, and proline, can help to promote cartilage synthesis and support collagen formation for healthy tendons, ligaments, and joints. For prevention and rehabilitation consider a natural, healthy shoe with a wide toe box, and flat and flexible sole. Correct Toes will additionally assist wide, splayed toes provide stability to the foot and ankle, facilitating arch strength, and helping to prevent excess eversion and inversion of the ankle. A thin, flat sole keeps the foot closer to the ground, maintaining a lower center of gravity within the foot, making it less likely to roll. The stronger and more stable your feet and ankle muscles and joints are, the less forces are translated to the knees and low back.

Regenerative Injection Therapy – for injuries and pains that are taking longer than expected to heal, consider regenerative injection therapies. These therapies activate the body’s self-healing mechanisms in order to heal damaged or degenerative tissues. Regenerative injection therapies recruit the growth factors and white blood cells that normally come to repair tissue from injury without reinjuring the tissue. This can strengthen tendons, repair ligaments, and regrow cartilage. Prolotherapy typically involves injecting dextrose (a sugar solution) into a problem area to trigger a local immune response, with the body sending immune cells and growth factors to the area, cleaning up damaged tissues in the process. It is important to have a robust immune system for this therapy to be successful. Platelet-Rich Plasma injections involve drawing blood, centrifuging it, and reinjecting the platelet-rich plasma, which is full of growth factors and platelets, directly into the problem area. This procedure is slightly more invasive but skips the step of having the body respond to an irritant, by directly injecting the platelets into the problem area. Stem Cell Therapy is a somewhat controversial therapy that involves injecting stem cells from one’s own bone marrow, one’s own adipose tissue, or from an external source such as amniotic fluid or umbilical cord. Stem cells are immature cells that provide a scaffolding to become many different types of cells, depending on the environment they are injected into. In a multitude of ways, regenerative injection therapies focus the body’s innate healing response in a specific area to induce rebuilding and regeneration.
Note: A cortisone injection is NOT a regenerative injection therapy. Cortisone is an anti-inflammatory steroid that shuts off the healing process in order to relieve pain. While pain relief can be helpful in the short term, unfortunately, cortisone often leaves the tissue weaker and more degenerated in the long term.
Basketball and Natural Footwear Options
Written by: Dr. Andrew Wojciechowski, ND
If you’re seeking more individualized foot health care and would like to work with Dr. Andrew directly, you can schedule at Northwest Foot and Ankle.
Schedule a virtual remote consultation with Dr. Andrew Wojciechowksi, ND.
Schedule an in-person appointment with Dr. Andrew Wojciechowski, ND at Northwest Foot & Ankle in Portland, OR.